Table of Contents
Medicaid is a publicly funded health coverage package for low-paid households with insufficient medical coverage. Each state offers Medicaid or a comparable program to assist pregnant women in obtaining proper antenatal and postpartum care. Medicaid also provides health coverage to older citizens, children, and those with ill health.
The federal government establishes the overall eligibility standards for Medicaid, though every government establishes its own particular eligibility rules, which might vary from state to state.

In the “fi” my in need” g” outing, pregnant women with incomes at or under 133 percent of the centralized poverty threshold will be included.
A pregnant woman may cover those who earn too much to qualify for the “fi” my in need” g” outing but fall within the “me”ically needy” c” category. This implies that females previously refused Medicaid eligibility may now be eligible. (Also known as increased Admissibility.)
Can I Get Pregnancy Medicaid if I Have Insurance?
Yes, you can get Pregnancy Medicaid if you already have insurance. To make the transition from your current insurance to Medicaid pregnancy coverage, you need to have the following documents in 2022:
- Evidence of pregnancy
- Evidence of citizenship for lawful US residents (Birth certificate or social security card serves as proof of identity.)
- Noncitizen ship proof if not a resident of the United States
- Proof of earnings
Medicaid eligibility is not as straightforward as it is for most other administration plans. Maximum management plans have explicit eligibility criteria and income restrictions to assist people in determining whether they meet the requirements.
However, there are other ways to qualify for Medicaid, and although income is one of the suitability criteria, it is not the only one. To be considered for Medicaid, limited-income persons must fall into one of the Medicare criteria.
Those with a moderate income may get ahead if they belong to any succeeding organizations and rely on other “co”t-sharing” a” arrangements (which function as a deductible before total insurance starts).
Suppose you are expecting and not covered by insurance. Contact the Medicaid office in your area to see whether Medicaid is your best choice.
What advantages does Medicaid provide to pregnant women?
Like other public health insurance systems, Medicaid does not provide members with direct financial benefits. Definite wellness professionals and health maintenance institutions have contracts through Medicaid to service Medicaid-insured patients. For Medicaid services, you should be given a list of local medical providers that take Medicaid or a website where you might seek a provider by location. If you get treatment as a Medicaid benefactor, your medical expenses will be reimbursed by Medicaid. (According to specific Medicaid laws and policies.)
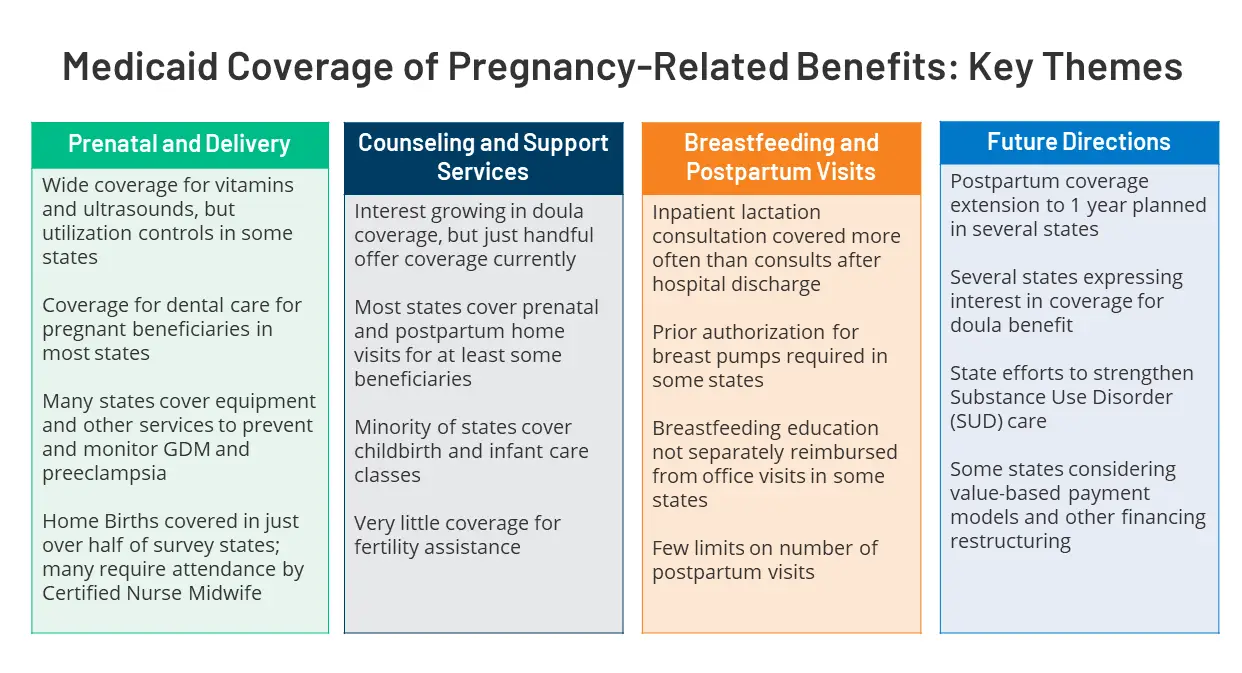
All care linked to pregnancy, birth, and any difficulties that may arise throughout the prenatal period and equal to sixty days after that are covered for pregnant women.
In addition, expecting women may be eligible for treatment they received during their pregnancy before applying for Medicaid. Certain countries call this “Os” sensible Admissibility, which is implemented to ensure that all pregnant women get antenatal precautions as early as feasible. Consult your confined administrative center to see whether you are eligible for presumed eligibility.
Expecting females are frequently given precedence in evaluating Medicaid suitability. Most offices attempt to determine a pregnant woman’s eligibility within 2 to 4 weeks. If you want medical care before then, consult your regional office for a temporary identification card.
Pregnant Women coverage: questions and answers
Historically speaking, being eligible for and enrolling in individual health insurance has been a prerequisite for having access to reasonably priced and increased, all-inclusive medical care throughout pregnancy. Because of the Patient Protection and Affordable Care Act (ACA), pregnant women can now access a broader range of medical treatment options. This Frequently Asked Questions document provides information on the treatment of healthcare facilities and services that unregistered women may use or be protected by Medicaid, the Marketplace, or independent or career coverage.
Medicaid for Women Who Do Not Have Health Insurance
- Is it possible for women without insurance coverage to participate in a government health insurance policy after they discover they are pregnant?
A pregnant lady who comes across the criteria for participation in Medicaid may join at any time throughout their pregnancy if they choose to participate in either program.
Medicaid covers all aspects of health care.
An expecting female is fit for complete Medicaid treatment at any stage of her pregnancy, provided that she satisfies the state’s state’s requirements. A few factors used to establish enrollment include family structure, average earnings, country of residency, and immigrant status.
A woman who does not have health insurance and is previously in the family way cannot participate in the Medicaid expansion if she applies during the open enrollment period.
Suppose a woman’s household income is higher than how much a family can afford to pay for Medicaid but is equal to or lower than the income limit for prenatal Medicaid in her state. In that case, she may be eligible for “pr”natal careora emblemspr”blems which may affect the deliv careM”dicare is included in this coverage. This is the case if the woman is expecting a child and has a condition that may make the pregnancy more difficult.
The revenue thresholds for receiving prenatal Medicaid benefits differ from state to state; nevertheless, states are prohibited from dropping entitlement from the federal poverty level (FPL) from 133 to 185 % of this covcoverage’sgal floor. States can establish a more significant minimum income requirement.
-
Does Medicaid provide comprehensive health care insurance to pregnant women?
However, this is not the case in every state. Complete coverage Medicaid offers inclusive analysis in each state, including all aspects of care throughout pregnancy, birth, and postpartum, as well as any additional medically needed treatments.
Services that are “es”ential on behalf of the wellbeing of a prenatal female or that have become needed as a result of the womwoman’segnancy” a”e covered by Medicaid when they are associated with pregnancy.
Because it is hard to decide which facilities are relevant to pregnancy because the motmother’salth is linked with that of the fetus, the breadth of covered treatments must be as broad as possible. A piece of federal legislation mandates Planned Parenthood and maternity care are also covered under the insurance plan, in addition to treatment for situations that might jeopardize carrying the pregnancy to a complete span. In addition, the legislation mandates therapy for conditions that may affect carrying the pregnancy to full term or the safe birth of the fetus. In the end, the state decides the extent of the covered services. Forty-seven states provide some Medicaid coverage for pregnant women, which is considered complete since it meets the requirements for the minimum required coverage (MEC). These guidelines dondon’tply to Arkansas, Idaho, and South Dakota; hence they arearen’tnsidered widespread.
-
How long does a woman remain eligible for Medicaid pregnancy coverage?
Regardless of whether or not there has been a change in financial circumstances, pregnant women continue to be eligible for Medicaid coverage throughout the postpartum period until the final day of the month, when their 60-day postpartum period ends.
As soon as the postpartum period ends, the state must investigate whether the woman is eligible for different Medicaid coverage categories.
-
Is it possible for a pregnant woman to get Medicaid care before it is established whether or not she is eligible?
Maybe. Some applicants for Medicaid, such as pregnant women, are eligible for “pr”sumptive eligibility,” w”ich means that their states have the option but are not required to provide it. [8] As a result of this provision, pregnant women can get quick, same-day Medicaid care, often at the same clinic or hospital where they submit their application for Medicaid assumed eligibility. At the moment, thirty states provide presumptive eligibility to women who are pregnant.
Suppose a woman has access to the wellbeing insurance provided by a family memmember’sb but has not enrolled for coverage under that plan. Would this affect her eligibility for Medicaid?
Whether or not an individual has access to employer-sponsored or other types of private health insurance does not affect Medicaid eligibility.
-
What is the Medicaid pricing requirement?
None. The Medicaid statute forbids states from collecting copayments, deductibles, or other comparable fees for pregnancy-related or pregnancy-complicating care, irrespective of the Medicaid membership class. HHS assumes that “pr”gnancy-related care” e”compasses all services ordinarily protected in the state-owned proposal, except the government justifies the designation of a particular treatment as not prenatal. However, states may levy monthly charges for expecting females with earnings over 150 percent of the federal poverty level and control for undesired medications.
-
Could immigrant women not covered by insurance get treatment via Medicaid?
Perhaps. Noncitizen immigrants who meet all other Medicaid entitlement supplies in their state may apply for Medicaid. Still, they must wait five years after obtaining their succeeding colonization rank before they may do so. Certain qualifying noncitizens are exempted from the 5-year limit since they are legal permanent residents. In 2010, the 5-year to come requirement was repealed for legally dwelling immigrants, providing states the choice to give legally living refugee females access to prenatal Medicaid irrespective of how long they had lived in the United States. Pregnant legal residents in 23 states are eligible for Medicaid coverage immediately. Federations may offer funded prenatal care to illegal immigrant women who are DACA-eligible or undocumented. Certain federations may also provide prenatal care funded totally by the state.
-
Does Medicaid cover abortions?
The Hyde Amendment, a yearly provision added to a federal appropriations bill by Congress, restricts the use of government money for abortion coverage unless a pregnancy is the result of rape or incest or if prolonging the pregnancy would threaten the womwoman’sfe.
However, governments can use their money to pay for abortions; now, 17 states do.
-
What changes are faced by pregnant women who are already registered in Medicaid?
Typically nothing. Pregnant women previously eligible for and registered in complete Medicaid will continue to be fit and have access to pregnancy care. A female who falls in the family way whereas registered in Medicaid Growth may maintain coverage until redetermination. For example, if a pregnant woman is eligible for prenatal Medicaid, the state has to let her know about the advantages she may qualify for under other categories of coverage.
-
Wilprotectotection to neonatal patients as well?
Yes. A neonatal born to a Medicaid-enrolled mother qualifies for considered neonatal protection. This coverage starts at delivery and continues for the year, independent of family income fluctuations.
-
What are the expenditures requirements in Medicaid?
See the section under “Po”sibilities for Uninsured Females in the Public Sector.”
- F”ll-coverage and growth Medicaid offers comprehensive health insurance for pregnant women.
Of course. Medicaid covers prenatal care, childbirth, the postpartum period, and any medically required treatments, whether or not they are unswervingly connected to pregnancy.
-
Does Health Insurance Marketplace plans ultimately offer coverage for women, plus motherhood precautions?
Yes. Motherhood and neonatal care must include one of the 10 Essential Health Benefits (EHBs) in all Covered market policies. The Department of Health and Human Services has not stated but should be included in this category, giving that power to the federations. Consequently, specific maternity care benefits differ by state.
-
What changes occur when a pregnant woman enrolls in a Marketplace strategy?
Nothing will happen until she tells it to. If she qualifies for Medicaid, the woman can choose to stay in her Marketplace plan or switch to one of these programs. If a woman has admittance to MEC via complete coverage or prenatal Medicaid, she will not be disqualified from receiving APTCs; nevertheless, she cannot participate in both programs simultaneously and must choose between them. The overall cost, the availability of preferred providers, the impact of switching plans, and the end product on private analysis all factor into the decision-making process.
- After giving birth, may a woman who previously had Medicaid reenlist in a Marketplace proposal if she is otherwise eligible?
Maybe. If the baby is entitled to Marketplace protection and a SEP, the mother may be able to re-enroll in Marketplace coverage.
- Is The Affordable Care ActAct’salth Insurance Marketplace not covering newborns?
Yes. The ACACA’s Provision necessitates prenatal and postnatal care coverage for women and their newborns. The maintenance of a newborn includes all aspects of the delivery process and the first few days of the baby’s life. Each state and plan will have specific requirements, but all new moms with Marketplace protection must enroll their infants as soon as they are born.
If the neonatal is suitable, the parents may choose to add the child to their existing marketplace proposal or purchase a new Marketplace plan specifically for the child.
If parents decide on the second option, they may enroll the youngster in any Marketplace plan. However, others in the family may be unable to change their present Marketplace coverage when enrolling a newborn.
-
Is Marketplace coverage for Abortion included?
Dependent on the idea, in various states. Health Insurance Marketplace plans cannot provide coverage for Abortion in 25 states. Total limits are imposed in two states, but Hyde exceptions are used in the other 23 jurisdictions. The rest of the federations have no limitations.
- Is maternity care included in insurance plans offered by employers or others outside the Marketplace?
It all depends. Employer-sponsored insurance is exempt from this duty.
- Is it possible for a woman to have Medicaid and private insurance?
Yes. one may use Medicaid in combination with a non-Marketplace private insurance plan by a woman who comes across MedMedicaid’srnings and suitability criteria.
- Is a newborn covered under a private health insurance policy?
It all depends on what youyou’reoking for. Employer-sponsored insurance is exempt from this duty. Regarding infant care, ladies should register their offspring in insurance coverage immediately after delivery.
- Does Abortion is covered by private insurance?
Liable on the plan in various states. Abortion handling in reserved healthiness insurance is restricted in ten states, whereas the rest do not.
Conclusion
Pregnant women have many health insurance options, making it difficult to go through them all. Pregnant women now have additional options for health insurance, thanks to the ACA. As soon as a low-income woman becomes pregnant, she is entitled to register in Medicaid and get inclusive healthiness carefulness facilities. In most cases, pregnant women currently covered by health insurance may keep it or apply for Medicaid. After the birth of a child, a womwoman’salth insurance options may change again, allowing her to switch to a new provider or return to an old one.
