When you visit a Walgreens pharmacy, you may encounter a pharmacist reviewing your prescription. This may seem like an inconvenience, but it is vital to ensuring your safety and medication effectiveness.
Pharmacists are highly trained medical professionals specializing in medications and their effects on the human body. They are responsible for verifying that all prescriptions are safe and appropriate for the patient, considering factors such as allergies, drug interactions, and overall medical history.
What does Walgreens’s delayed pharmacist reviewing prescriptions mean?
If you see a message that Walgreens Pharmacist Reviewing Prescription, it usually means they are out of stock or have to verify the medication with the doctor. If they are out of stock, in 24 hours, they will get medicine in most cases.
The process of reviewing a prescription can involve several steps. First, the pharmacist may consult the prescribing doctor to clarify dosages or medication instructions. They may also need to check the patient’s insurance to see how much of the medication is covered and whether prior authorizations are required. The pharmacist will also inspect the drug, checking for any physical defects or inconsistencies.
There can be several reasons why people may experience delays in getting their prescriptions filled at Walgreens or any pharmacy. However, here are some of the most common reasons why medication may be delayed or take longer than expected to fill:
- Incomplete or illegible prescription: If a drug is vague or unclear, the pharmacy may need to contact the prescriber for clarification or additional information, which can delay the prescription.
- Manufacturer back orders: Occasionally, the medication manufacturer may experience a shortage or delay in producing the drug, which can result in back charges. When this happens, the pharmacy may be unable to fill the prescription immediately and may need to wait for the medication to become available.
- Medications requiring prior authorization: Some drugs require prior approval from the insurance provider before being filled out. This means the pharmacy must obtain permission from the insurance company before filling the prescription. This process can take several days and may delay the filling of the drug.
- The high volume of prescriptions: During busy periods, such as flu season or after holidays, the pharmacy may experience a high volume of drugs to fill. This can result in longer wait times and delays in filling prescriptions.
- Insurance issues: If there are issues with the patient’s insurance coverage, such as a change in coverage or a lapse in coverage, this can result in delays in filling the prescription.
Filling prescriptions can frustrate patients, but it is essential to understand that many factors can contribute to these delays. To minimize the chances of experiencing delays, it is necessary to ensure that prescriptions are complete and legible, allow plenty of time for the pharmacy to fill the drug, and work with the pharmacy and insurance provider to resolve any issues.
If the pharmacy does not have the medication in stock, the pharmacist will place an order to have it delivered. This can sometimes cause a delay, but waiting for the drug to arrive is essential rather than trying to substitute another medication. Switching medications can have unintended consequences and could potentially harm the patient.
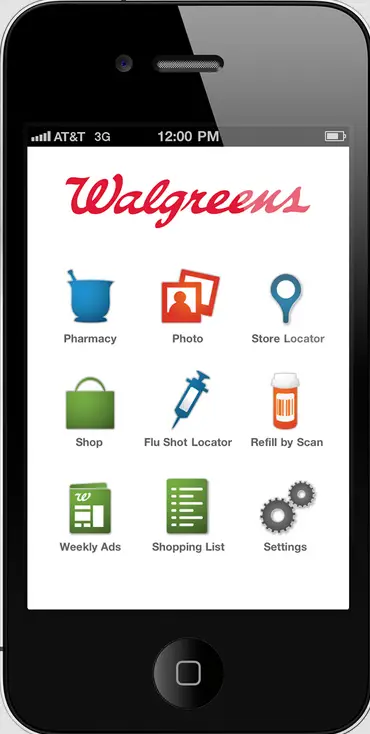
In addition to reviewing prescription medications, Walgreens pharmacists provide various other essential services. For example, they can administer vaccinations, advise on over-the-counter medicines, and help patients quit smoking. Walgreens pharmacists are dedicated to helping patients achieve better health outcomes by providing high-quality care and personalized attention.
So, if you are waiting for a pharmacist to review your prescription at Walgreens, remember that this is an essential step in ensuring your safety and well-being. By reviewing your prescription carefully, Walgreens pharmacists are committed to providing you with the best possible care.
Insurance issues at Walgreens
Insurance issues can be a common reason patients may experience delays or difficulties getting their prescriptions filled at Walgreens or any pharmacy. Some of the most common insurance issues that can arise include:
- Changes in insurance coverage: If a patient’s insurance coverage changes, such as switching to a new plan or insurance provider, this can sometimes result in delays in filling prescriptions. The pharmacy may need to verify further insurance coverage and obtain necessary approvals before filling the prescription.
- Lapse in insurance coverage: If a patient’s insurance coverage lapses due to non-payment or for another reason, this can result in difficulties in filling prescriptions. The pharmacy may need to verify the patient’s coverage status and obtain necessary approvals before filling the prescription.
- Prior authorization requirements: Some medications require prior authorization from the insurance provider before being filled out. This means the pharmacy must obtain approval from the insurance company before filling the prescription. If the insurance company requires additional information or documentation, this can result in delays in filling the prescription.
- Coverage limitations: Some insurance plans may limit coverage for certain medications or require the patient to pay a higher copay for specific medicines. If a patient is unaware of these limitations or is not prepared to pay the higher copay, this can result in difficulties in filling the prescription.
- Coordination of benefits: If a patient has multiple insurance plans, such as primary and secondary insurance, the pharmacy may need to coordinate benefits between the two programs before filling the prescription. This can result in additional paperwork and delays in filling the prescription.
