Table of Contents
Many abbreviations and acronyms are used in health insurance, which can confuse the uninitiated. One term you might encounter on your insurance card is “PCN.” PCN stands for Processor Control Number, which is crucial in how your insurance company handles your medication benefits.
What is PCN on an Insurance Card?
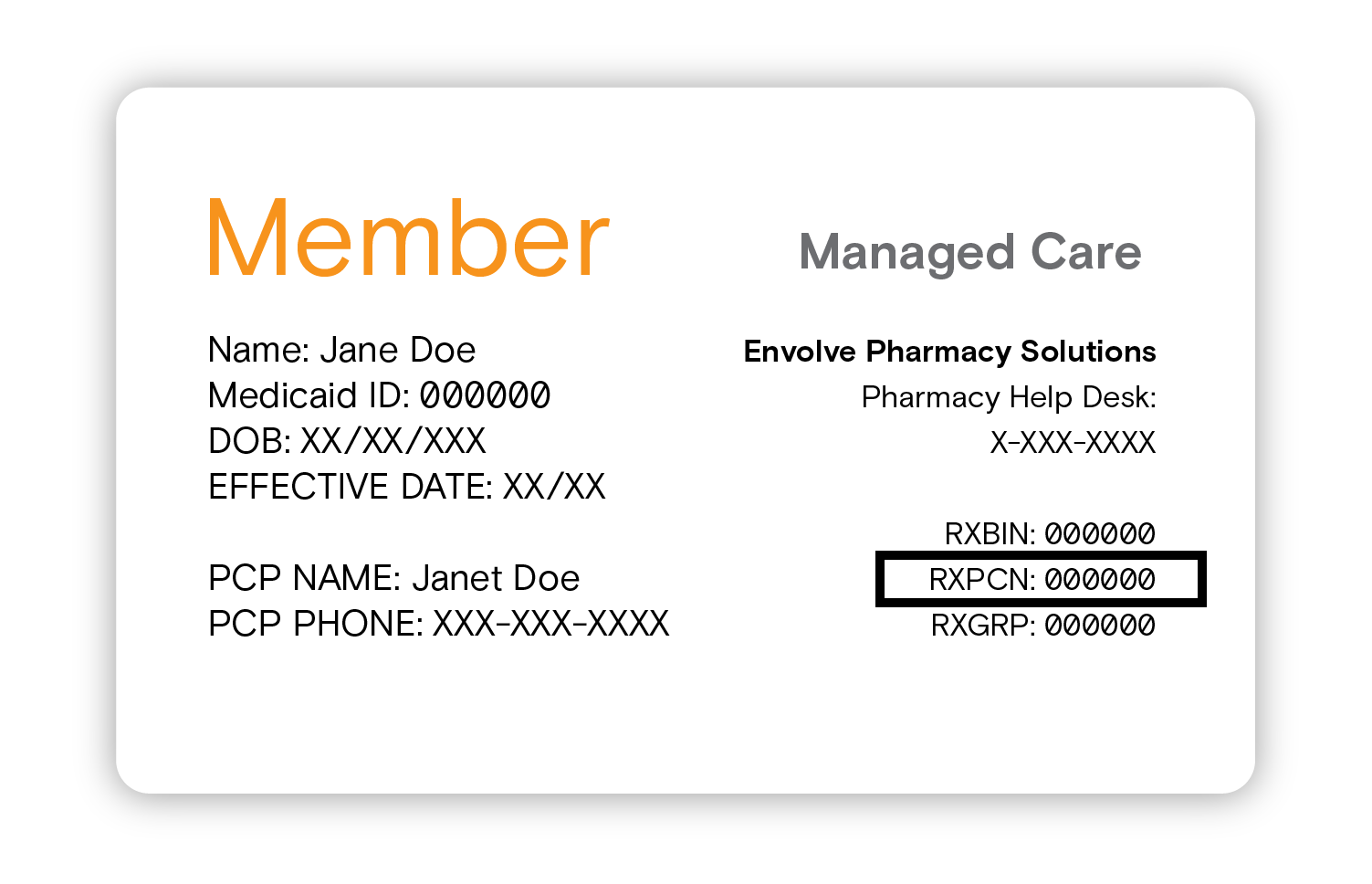
PCN, or Processor Control Number, is an identifier insurance companies use to route pharmacy transactions for prescription benefits. The number is typically found on the front of an insurance card, alongside other vital information, like the member ID, group number, and Rx BIN (Bank Identification Number).
Insurance companies have contracts with pharmacy benefit managers (PBMs), which administer prescription drug programs. The PCN assists in correctly routing the claim to the appropriate PBM, which can then process it according to the policy’s benefits and coverages.
The PCN serves as a second identifier that helps the pharmacy and the PBM ensure the correct claim processing.
PCN and Rx BIN
The PCN works in tandem with the Rx BIN. The BIN helps pharmacies process prescription benefits with PBMs, identifying the precise PBM for each claim. While the BIN is the primary identifying number, the PCN can be considered a secondary identifier. Sometimes, a PBM might manage several different health plans, and the PCN helps distinguish between those plans.
PCN (Processor Control Number):
- The PCN is a secondary identifier used by insurance companies.
- It is primarily used to correctly route pharmacy transactions for prescription benefits.
- PCN helps identify the plan details within the PBM, allowing for the correct claim processing.
- Not all insurance cards have a PCN. In such cases, the pharmacy might use a default or standard PCN.
- If your card doesn’t have a PCN, call your health insurance company or the pharmacy benefit manager to get this information.
Rx BIN (Bank Identification Number):
- The Rx BIN is a primary identifier used by pharmacies.
- It routes the claim to the correct Pharmacy Benefit Manager (PBM).
- The BIN helps pharmacies process prescription benefits with PBMs, identifying the precise PBM for each claim.
- Every insurance card will have an Rx BIN.
- The Rx BIN is critical in ensuring your pharmacy can bill your prescription to your insurance company correctly.
How is the PCN used?
When you go to a pharmacy to fill a prescription, the pharmacist enters your Rx BIN, PCN, member ID, and group number into their system. This information allows the pharmacy to communicate with the correct PBM, verify the insurance coverage, determine the amount to be paid by the insurance company and the patient’s co-pay, and check other details like approved medication quantities or refill frequencies.
PCN we can use in the following ways:
- Pharmacy Identification: When you visit a pharmacy to fill a prescription, the pharmacist uses your PCN to identify the correct insurance plan details and route the claim appropriately.
- Claim Routing: The PCN serves as an additional identifier insurance companies use to correctly route pharmacy transactions for prescription benefits to the appropriate Pharmacy Benefit Manager (PBM).
- Insurance Verification: The PCN, in combination with other details like the Rx BIN, member ID, and group number, enables the pharmacy to communicate with the correct PBM. This communication helps verify insurance coverage, ensuring the policyholder has the appropriate benefits to cover the medication.
- Payment Determination: With the PCN, the pharmacy system can determine the amount the insurance company will pay and calculate the patient’s co-pay.
- Medication Details Verification: The PCN also helps the pharmacy and PBM to check details like approved medication quantities, refill frequencies, and whether prior authorization is needed for certain medications.
- Health Plan Differentiation: If a PBM manages several different health plans, the PCN helps distinguish between those plans, ensuring that claims are processed according to the correct plan’s rules and coverage.
Do all insurance cards have a PCN?
Not all insurance cards have a PCN. Some cards will only have the Rx BIN, enough for the PBM to process claims. In such cases, the pharmacy might use a default or standard PCN. However, it is best to provide all the information on your insurance card when you go to the pharmacy to avoid confusion or miscommunication.
What do you do if your card doesn’t have a PCN?
If your insurance card doesn’t have a PCN (Processor Control Number), you can follow these steps:
Step 1: Don’t panic. Not all insurance cards include a PCN. It’s possible that your insurance provider or pharmacy benefit manager (PBM) does not use a PCN to process pharmacy transactions. They might use the Rx BIN (Bank Identification Number) or another method.
Step 2: Double-check your insurance card. The PCN might not be marked as such. It could be listed under a different heading or included in the string of numbers and letters that make up your member ID or group number.
Step 3: Contact your insurance provider. Their contact information is usually on the back of your insurance card. Ask them if your plan uses a PCN and, if so, what it is.
Step 4: Call your pharmacy benefit manager (PBM). If your insurance company cannot provide a PCN, your PBM should be able to. The PBM is the organization that manages your prescription drug benefits. Your insurance card should also have the PBM’s contact information.
Step 5: Provide the PCN to your pharmacist. Once you’ve obtained your PCN, be sure to provide it to your pharmacist the next time you fill a prescription. This will ensure that your pharmacy transactions are processed correctly.
Step 6: Update your records. Once you have this information, it might be helpful to write it down and keep it safe for future reference.
Remember, the process might differ slightly depending on your specific insurance provider, but these steps provide a general guide.
Call your health insurance company or the pharmacy benefit manager if you can’t find your PCN. They should be able to provide you with the number. Also, remember that it’s common for many insurance cards to include a PCN, but it’s not mandatory. Some insurers might not use a PCN at all, and that’s okay.
Conclusion
Navigating health insurance can sometimes be daunting, given the plethora of terminology. However, each piece of information, like the PCN, ensures the insurance process runs smoothly. Understanding what a PCN is and its role can help you better manage your pharmacy transactions and streamline your healthcare experience.
